An independent review has revealed a lack of accountability, openness and transparency in Jersey's Health Department - and warned that there'll be some substantial and noisy opposition to changing that.
The review of quality and safety in the hospital also found instances of bullying by doctors, constructive advice being dismissed and an unwillingness from executives to hold 'powerful and well-connected' minorities to account.
"Some reported good team working both with and between doctors. However, a disconcerting number reported poor working relationships including bullying by doctors or a lack of assertiveness of nurses, or both."
Professor Hugo Mascie-Taylor carried out 77 interviews with 53 people during seven visits to Jersey.
The most used phrase by the 53 interviewed was that 'there are no consequences' and that incidents are not reported by staff because they are reluctant - with some fearing they'd be punished for it.
Many think the executive are trying to deal with some of the problems, but they're not confident it will succeed. They're more confident of losing their jobs if they pushed too hard for improvements.
Those who described examples of poor behaviour, such as bullying, feel that they're not reported because of the perception that nothing will be done about it.
The culture has been described as non-accountable and individualistic, with some groups of staff seeing change as 'unnecessary, interfering, bureaucratic and certainly not required in Jersey.'
The phrase 'The Jersey Way' was used to critically describe the culture. The reviewers say that's potentially highly damaging to patient care.
It reveals that some staff are resistant to transparency, as they feel it's either unnecessary or bureaucratic interference.
The review team have called on the government to lead assertively when it comes to coping with any fierce reaction.
The areas most pointed towards when it came to accusations of poor behaviour, such as bullying, were theatres and some wards.
"This behaviour is at best undermining and, at worst, potentially unsafe.
Most concerning was that those describing these examples of poor behaviour at interview felt that they were not reported because of the perception that no action, disciplinary or otherwise, would occur.
In fairness it was also widely recognised that HCS is making tangible efforts to improve this situation but that changing a long-established culture is very challenging."
A point made regularly by those interviewed was that the problems are 'deep-seated and historic' and reflect longstanding wider societal traits.
"For those who had arrived more recently, in the last decade or so, there was surprise expressed that so little positive change had occurred before or since their arrival.
"Those who have been in Jersey longer expressed similar sentiments but sometimes saw the lack of change as a strength rather than a weakness. Whilst many did not welcome the situation, others did, or were resigned to it.
HCS does not appear to have been proactively managed in the past, perhaps for decades."
The reviewers also found a reluctance to follow national guidelines - such as the National Institute for Health and Care Excellence (NICE).
Some said "it might well work elsewhere but it would not work here,” or “it couldn’t work here.”
There is a failure to place performance information in the public domain, which the review team say neglects a powerful driver of safety and quality improvement.
"Arguments were advanced by some interviewees that the data is insufficiently robust, or that the public would be alarmed if the data were revealed to them.
The way to improve the quality of the data is to make it clear that it will be put in the public domain.
The public has the right to know about the quality of the services provided by HCS."
There are also accusations that private patients are prioritised over public patients.
Alleged examples include:
- Private patients being seen more frequently by their consultant
- Private patients more likely to be labelled urgent than public patients with the same condition (and therefore receiving treatment more quickly)
- The procedures being more likely to be undertaken by a consultant if the patient is a private patient and more likely to be undertaken by a less trained doctor if the patient is a public patient (which does not necessarily mean that it is unsafe)
- That consultants sometimes absent themselves from the care of public patients to provide care for private patients,
- Private patients are advantaged by being placed first on lists and are therefore more likely to be done by the Consultant and less likely to be cancelled.
"Whilst interviewees inevitably had differing views about the frequency of these difficulties there was little dispute that at least some of them occur some of the time.
It is not an ideological point to recognise that if some or all the allegations above are true, then there is a potential direct effect on patient safety and the quality of care. There may also be an undermining effect on teamwork."
61 recommendations have been made to improve care.
They include:
- The government should hold the Health Department to account in a more rigorous and robust way.
- Executives should act with courage and with a strong focus on the patient, not the protection of individual members of staff.
- The Health Department should act assertively to deal with poor and unprofessional behaviour.
- The Health Department and executives should recognise that they have a joint responsibility for the safe care of all patients, both public and private, in the hospital.
- Put more information about performance in the public domain.
- Make it clear that a failure to report incidents is unacceptable to the organisation and is unprofessional. Make it abundantly clear that those reporting incidents will be protected from any form of intimidation and that anyone attempting to stop reporting will find themselves in serious difficulty.
- Evaluate alleged intimidatory behaviours and take clear and measurable remedial action if needed.
- Develop and publish a mandatory training policy and insist that employees complete it. If they fail to comply, they will be held to account.
- Assure itself that the management of patients is equitable and equally safe for all.
In response to this scathing report, Health Minister Deputy Karen Wilson has announced that an independent health board will be created.
"Islanders will rightly expect that, as the new Minister for Health and Social Services, I will ensure that urgent, clear and direct action is taken to address the report’s recommendations. Our health service must become an exemplar of safe and effective care, be of good quality, and its performance accounted for in an open and transparent way.

In light of this, I will bring forward plans to establish an independent health board, including experts in health care provision, to drive reform, improve governance and address the cultural, structural and practice issues affecting the quality and safety of the care provided.
Alongside that Board, I will strengthen policy functions to determine government policy across the whole health system."
She has ordered an immediate turnaround plan for the hospital while the new independent board is created, with a follow-up review scheduled for a year's time to track progress.
The independent review was commissioned by the Health Department's Director General, Caroline Landon.
That was at the request of Medical Director Dr. Patrick Armstrong and Chief Nurse Rose Naylor.
All 61 recommendations have been accepted.
A Q&A from the Health Department's Executive Team has been published alongside the independent report.
Q: How do you see the behaviour of some staff as described in the report, do you think it is fair?
A: Our values are very clear. No kind of behaviour which makes another colleague feel de-valued or upset is acceptable, irrespective of their title, grade or length of service. Every HCS colleague deserves equal treatment by every other HCS colleague.
Q: How are you going to bring about changes in staff culture?
A: The improvement will be led by the staff in the services, it is their culture. This needs to be supported by the clear lines of accountability, which will allow clarity of roles and responsibilities. We will have clear expectations of professional standards and conduct that will be required in the organisation. We expect civility in all interactions.
Q: Are consultants being allowed to prioritise private patients?
A: All patients are prioritised according to clinical need. In a number of areas, we have separated public and private patient activity. One of the key messages from the report is the need for the Government to provide clear policy direction on the delivery of public and private activity.
Q: Why doesn’t Jersey follow NICE guidelines and practice?
A: Historically there has been no expectation to follow or assurance around the evidence base that has been used. Despite this, there are areas across HCS of good practice, however there are examples of individual clinician decisions without the appropriate measures and benchmarks in place and without the governance structures in place to check it has been appropriate. This is part of the journey we are on. Our aspiration is to follow robust evidence base in all we do.
Q: Have islanders’ lives been put at risk by the findings identified in this report?
A: Healthcare carries inherent risks. The findings of this report assist us in identifying the areas for us to mitigate those risks and improve care.
Q: Why isn’t data on clinical outcomes and performance publicly available? Will you make it available?
A: Our aspiration is to produce individual outcome data but this relies on continued investment in our informatics infrastructure.
"I commissioned this review to ensure clear and full understanding of what needs to be done to improve the Department’s quality, safety and governance arrangements. Professor Mascie-Taylor’s report does that. It sets out the extent of the challenge, and the necessary action required.

I want to thank those colleagues who participated in the review. Their willingness to be frank and open and freely give their views, even when doing so meant highlighting poor practice in some of their services, took courage.
Now that the report is published, and the issues are known, we can set about improving our clinical governance arrangements in order to advance the quality and safety of our services." - Caroline Landon.

 Civil Service recruitment freeze extended
Civil Service recruitment freeze extended
 DFDS brings in replacement ship for Portsmouth sailings
DFDS brings in replacement ship for Portsmouth sailings
 100 days until Orkney Island Games begin
100 days until Orkney Island Games begin
 £200k padel facility coming to Les Ormes in May
£200k padel facility coming to Les Ormes in May
 Two islanders trapped in a lift rescued from sixth-floor fire on the Esplanade
Two islanders trapped in a lift rescued from sixth-floor fire on the Esplanade
 Rooftop bar, climbing wall and concert hall in £110m Fort Regent plans
Rooftop bar, climbing wall and concert hall in £110m Fort Regent plans
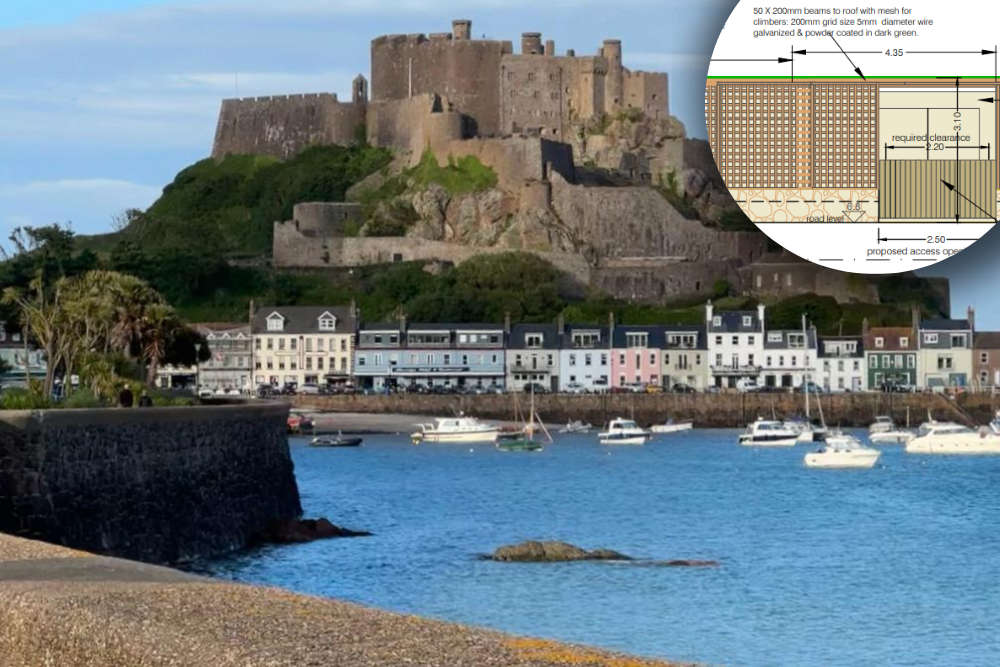 3m tall substation and bin store proposed for Gorey promenade
3m tall substation and bin store proposed for Gorey promenade
 European visitors now need permit for UK entry
European visitors now need permit for UK entry